Ali Oliashirazi
Marshall University, USA
Title: How to manage persistent draining wounds after total joint arthroplasty

Biography:
Dr. Ali Oliashirazi is Professor and Chair of the Department of Orthopaedic Surgery at Joan C. Edwards School of Medicine at Marshall University. He is also the Vice Dean for business development and external affairs at the School of Medicine. Dr. Oli, as his patients affectionately called him, graduated from George Washington University School of Medicine, where he was the valedictorian of his class. He completed his orthopedic training at the prestigious Mayo Clinic in Rochester, Minnesota. His passion and expertise is joint replacement surgery, in particular knee replacement surgeries. He lectures extensively, and his research has been presented both nationally and internationally. Dr. Oliashirazi is a board certified orthopaedic surgeon who is a Fellow of the American Academy of Orthopaedic Surgery and a Member of the American Association of Hip and Knee Surgeons.
Abstract:
Introduction:
Persistent wound drainage has been recognized as one of the major risk factors of periprosthetic joint infection (PJI). Currently, there is no consensus on the management protocol for patients who develop wound drainage after total joint arthroplasty (TJA). The objective of our study was to describe a multimodal protocol for managing draining wounds after TJA and assess the outcomes.
Methods: We conducted a retrospective study of 4,873 primary TJAs performed between 2008 and 2015. Using an institutional database, patients with persistent wound drainage (>48 hours) were identified. A review of the medical records was then performed to confirm persistent drainage. Draining wounds were first managed by instituting local wound care measures. In patients that drainage persisted over 7 days, a superficial irrigation and debridement (I&D) was performed if the fascia was intact, and if the fascia was not intact modular parts were exchanged (Figure 1). TJAs that underwent subsequent I&D, revision surgery, or developed PJI within one year were identified.
Results: The overall rate of persistent wound drainage was 6.2% (302/4,873). 65% (196/302) of patients with draining wounds did not require any surgical procedures. Of the patients with persistent drainage, 9.8% underwent I&D and 25.1% underwent revision arthroplasty. Moreover, 15.9% of these patients developed PJI within one year. Compared to those without wound drainage, TJAs complicated by wound drainage demonstrated an odds ratio of 16.9 (95% CI: 9.1-31.6) for developing PJI, and 18.0 (95% CI: 11.3-28.7) for undergoing subsequent surgery.
Conclusions: Wound drainage after TJA is a major risk factor for subsequent PJI and therefore, proper management of these patients has paramount importance. Our results demonstrated that drainage ceased spontaneously in 65% of the patients with local wound care measures alone. Wounds with persistent drainage were at substantially higher risk for PJI than those that healed uneventfully.
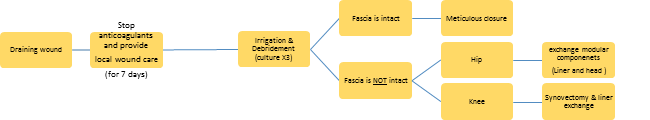
Figure 1 Management protocol for wound drainage after total joint arthroplasty