Diana Hodgins
European Technology for Business Holdings Ltd, UK
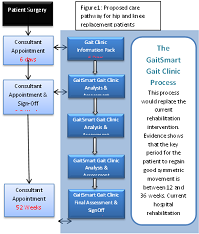
Title: Changing the care pathway for hip and knee replacement patients

Biography:
Diana obtained her degree in Mechanical Engineering and her PhD in solid state gyroscopes from the University of Hertfordshire (UH). Diana has 30 patents granted on solid state sensors and more recently on medical applications relating to the use of these sensors. In 2000 Diana was awarded an MBE for services to SMEs in the region and in 2002 she won the Women Inventor of the Year Award for Industry. In 2005 Diana was awarded an Honorary doctorate from the UH for services to innovation. In 1995 Diana and her husband established their own business, and in 2009 launched their sensor based gait monitoring product, GaitSmart. This system is now in use in variety of healthcare and sports applications. One of the sectors where it is applied is orthopaedics, with a particular focus on osteoarthritis and a number of papers have been published on this topic. Diana is currently a visiting professor at the UH and helped to establish a new MEng course in Biomedical Engineering and in 2014 was awarded Alumni of the year at the UH.
Abstract:
People with late stage hip or knee osteoarthritis may receive a joint replacement to relieve pain and improve mobility. The operation is considered a success, with regard to patient reported outcomes. However, studies using GaitSmart on hip and knee replacement patients one year post op show that less than 50% return to a normal gait and that these gait deficiencies can result in osteoarthritis in other joints, poor mobility and even falls if not corrected. People adapt their gait due to pain in the arthritic joint. Once the joint pain is gone, the patient needs retraining to walk correctly and weakened muscles strengthened. The current care pathway provides patients with physiotherapy for up to 6 weeks post op, guiding the patient to move the joint and become mobile. However, as it takes 10 weeks for the process of muscle strengthening to start, patients are signed off before gait retraining can really start. Patients are unaware of how they have adapted their gait; for example, excessive medial-lateral movement of the thigh i.e swinging the leg around the body rather than under the body. Therefore, the walking pattern remains the same, loading other joints incorrectly and poor use of their muscles. This paper proposes a new care pathway for patients, where gait kinematics are measured in the outpatient clinic using inertial sensors. A report describing the gait deficiency and the severity, using simple traffic light coding, together with a personalised exercise programme is provided to the patient at the end of their 15 minute session. Tests performed at 6, 12, 24 and 52 weeks post op monitor progress and allow the exercises to become more demanding as the patient improves. Evidence of the clinical efficacy of this approach will be presented.